Menière's Syndrome
As per our experience, the vascular system and its influence under sympathetic and parasympathetic stimulations plays an essential role in neurophysiology of equilibrium.
Every modification of arterial calibre, wherever it may be located at peripherical or central level, depending on sympathetic system may produce nutritional troubles at celular level with alterations in their functions.
These changes can be due to vasodilating phenomena as it is the case of hypotension or to arteriole spams, as it is the case of hypertension.
Menière, in his thesis published in 1861, describing the Syndrome or “Menière's Disease” has already mentioned these vascular alterations and has already connected them, in some cases, with migraine pathologies.
These facts have been our main reason to investigate, as from 1983, cerebral haemodynamics changes in patients with presumed diagnose of “Menière's Disease or Syndrome”, being our first edition “Über die Vaskuläre Migräne unter dem Ercheinungbild eine Menière Syndrome”.
At our Otoophtalmological Neurophysiology Data Bank with 7800 patients, 51% consult on a Menière kind syndrome joined to neurovegetative symptoms. In this group, 54% show migraine or headache background while 10% present diplopia or double vision.
The releasing mechanism consists, in 55,8% of the cases, of postural modifications and in 31.1% of kinetosys.
These patients have been under investigation by means of:
Equilibriometrical Examination
General statistics of the tests show the following results:
| 30.44% | central vestibular pathology of brainstem |
| 28.44% | central vestibular pathology of brainstem and cortical |
| 16.78% | central cortical vestibular pathology |
| 12.98% | peripherical vestibular pathology |
| 11.80% | combined peripherical and central vestibular pathology |
Cerebral Haemodynamic Examination
92% of patients showing compatible symptomatology with Menière Syndrome presented haemodynamic pathology which could be objectified.
55.5% with central vestibular lesions show spastic haemodynamic disorders and 33.2 % vasodilating haemodynamic disorders, 11.3% some other presentations.
75.22% of patients showing compatible symptomatology with a Menière present central vestibular lesions or dysfunctions which can be qualitatively and quantitavely objectified by means of the aforementioned numerous neurophysiological measuring methods.
Only 13% of the patients present a plain peripherical pathology compatible with a Menière Disease which can be qualitatively and quantitatively objectified, being the etiopathogenesis in 92% produced by haemodynamic disorders and only in 8% of the cases the etiopathogenesis has been produced by some other reasons, which could be infectuous, toxic, metabolic, etc.
As first and main step, it should be avoided any confusion in diagnosis and therapy, i.e. treating every patient presenting the very well known Menière trilogy (vertigo, hypoacousia, tinnitus) as a simple lesion of the inner ear without taking into account that the equilibrium system is something more complicated than a semicircular canal, where it does not only exist a ear and an auditive nerve, disregarding organs and most important vias as: brainstem, cerebelum, thalamus-cortical projection via, cerebelum-oculomotor via, cortical and cognitive vestibular areas, etc. Any alteration in neurotransmission in this complex of nucleus and vias will produce a Menière like Syndrome, together with or without any other symptoms.
It should be bore in mind that only in 13% of the cases, we can be in front of a true Menière Disease or Hydrops on which the specific treatment of it will suceed.
Advances in basic research in neurosciences and the introduction of new non-invasive techniques, that make possible the detection of weak signals of the brain, improving diagnosis and treatment of the Menière Syndrome.
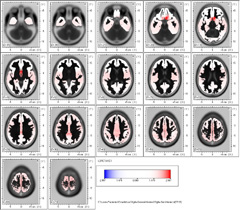
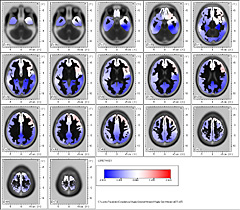
We use at our laboratory Otoohtalmological Neurophisiology, Buenos Aires, Argentina – Dr. med. G. Bertora and Dr. med. J. Bergmann – the EEG register in 21 derivation channels. The use of a specialized software Low Resolution Brain Electric Tomography – LORETA-. (Pascual-Marquí et al., 1994) makes possible obtaining functional imaging of the brain in 2D and 3D.
For instance, the cortex can be modeled as a collection of volume elements of 2394 voxels in the digitized Talairach atlas provided by the Brain Imaging Center, Montreal Neurological Institute.
In 2004, we carried out at Otoneuroohtalmological Neurophisiology, Buenos Aires, Argentina – Dr. med. G. Bertora and Dr. med. J. Bergmann – a comparative study using Low Resolution Brain Electric Tomography (LORETA) among 85 patients who have consulted on: Menière Syndrome and the results were compared vs. 390 patients from our Data Bank.
In Menière Syndrome we could see Delta low frequency band, in 1.75 Hz. An outstanding frontalization is observed comprising Brodmann areas 25, 38 and 10.
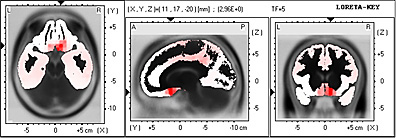
In 3D representation and in Talairach Atlas, it is observed that they bilaterally comprise the Medial Frontal Gyrus.

In ßeta 1 Band in 13.25 Hz frequency, frontalization remains in these patients comprising Brodmann areas 13, 47 and 45.
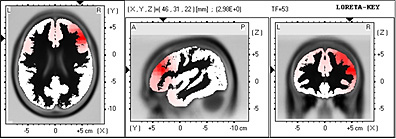
In Talairach Atlas and in 3D representation, it is observed the left prevalence of Frontal Inferior Lobe, Insula and Sublobar region.
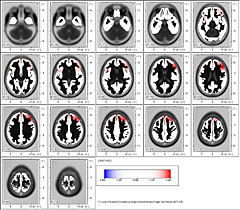

In ßeta 2 Band in 21.75 Hz frequency the exclusive location of dipole in Brodmann area 36 is highly significant.
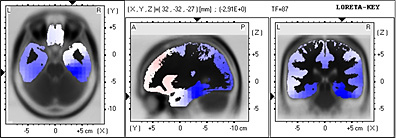
Which comprises the Limbic Lobe and the Parahippocampal gyrus left

Summing up:
The Menière Syndrome – vertigo, hypoacusis, tinnitus – has an important cortical representation in:
- Lóbulo frontal – Area de Brodmann 25
- Lóbulo Límbico
- Gyrus Parahipocampal
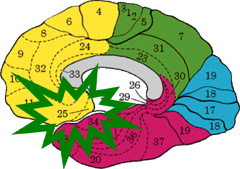
- Frontal areas Brodmann 25
- Limbic Lobe
- Parahippocampal Gyrus.
Our investigation (Bergmann – Bertora, 2004) capable of proving the fact that the Brodmann area 25, subgenual area and parahypocampal gyrus are involved in the Menière Syndrome has not been described yet in international bibliography.
This study allows us to open the black box of the Menière Syndrome.
The reason why the exclusive treatment of the peripheral organ and / or of the vestibular and auditory dysfunction does not lead to the whole and absolute compensation of the affection in many patients, is due to the fact that the prefrontal cerebral dysfunctions which always maintain latent this pathology are not being treated.
The frontalization present in all these patients and the involvement of the limbic lobe and prefrontal lobe is extensively demonstrated in Menière. But, there is a highly significant interindividual variation where different types of cerebral rhythms can be combined, which definitely indicate a hypofunction or hyperfunction of some neurotransmitters.
Our research and publications
- Archives for Sensology and Neurootology in Science and Practice. ASN
Volume 2 - 2004
Menière Syndrome and Vestibular Migraine: Cortical Brain Projections
Dr.med. Guillermo O. Bertora, Dr.med. Julia M. Bergmann (Buenos Aires - Argentina) - Archives for Sensology and Neurootology in Science and Practice. ASN
XXXIII Congress of the NES – Bad Kissingen – Germany – Page 2 – 2006
Menière Syndrome: Cortical Brain Projections studied by Brain Electric Tomography (LORETA)
Dr.med. Guillermo O. Bertora, Dr.med. Julia M. Bergmann (Buenos Aires - Argentina) - Archives for Sensology and Neurootology in Science and Practice. ASN – ISSN 1612 – 3352
XL Congress of the NES – Bydgoszcz – Poland – April 2013
Menière Disease – Is it a special sort of Migraine? Our experience
Dr.med. Guillermo O. Bertora, Dr.med. Julia M. Bergmann (Buenos Aires - Argentina)